Could Nanoparticles Mark a Breakthrough in Cancer Research?
Researchers of Karlsruhe Institute of Technology (KIT), Max Planck Institute for Multidisciplinary Sciences, and University Medical Center Göttingen have developed a groundbreaking method to treat pancreatic cancer more effectively and with fewer side effects in future. The new treatment approach uses tiny nanoparticles that deliver drugs directly targeted to cancer cells. This could mark a breakthrough in cancer research.
Pancreatic cancer is one of the deadliest types of cancer. It is often detected very late, as the early stages of the disease rarely cause symptoms or pain. Conventional treatment methods such as chemotherapy with so-called cytostatics are often not sufficiently effective and damage healthy tissue. This leads to major side effects and a reduced quality of life of the patients.
Issue 2024/2 of the lookKIT research magazine deals with methods and technologies to improve health care.
To the MagazineFor some ten years now, chemical, biological, and medical researchers led by Professor Claus Feldmann and Professor Frauke Alves have been working on a solution. Their idea: Targeted cancer therapy using smallest nanoparticles.
Feldmann’s research group at KIT’s Institute for Inorganic Chemistry has specialized in the development of new materials for medical applications. Renowned cancer expert Alves heads an interdisciplinary working group at Max Planck Institute for Multidisciplinary Sciences and University Medical Center Göttingen. In close cooperation, the researchers have come closer to a solution. First tests have been completed successfully and the next steps will show whether the new method will keep its promises.
Nanobus for Targeted Therapies
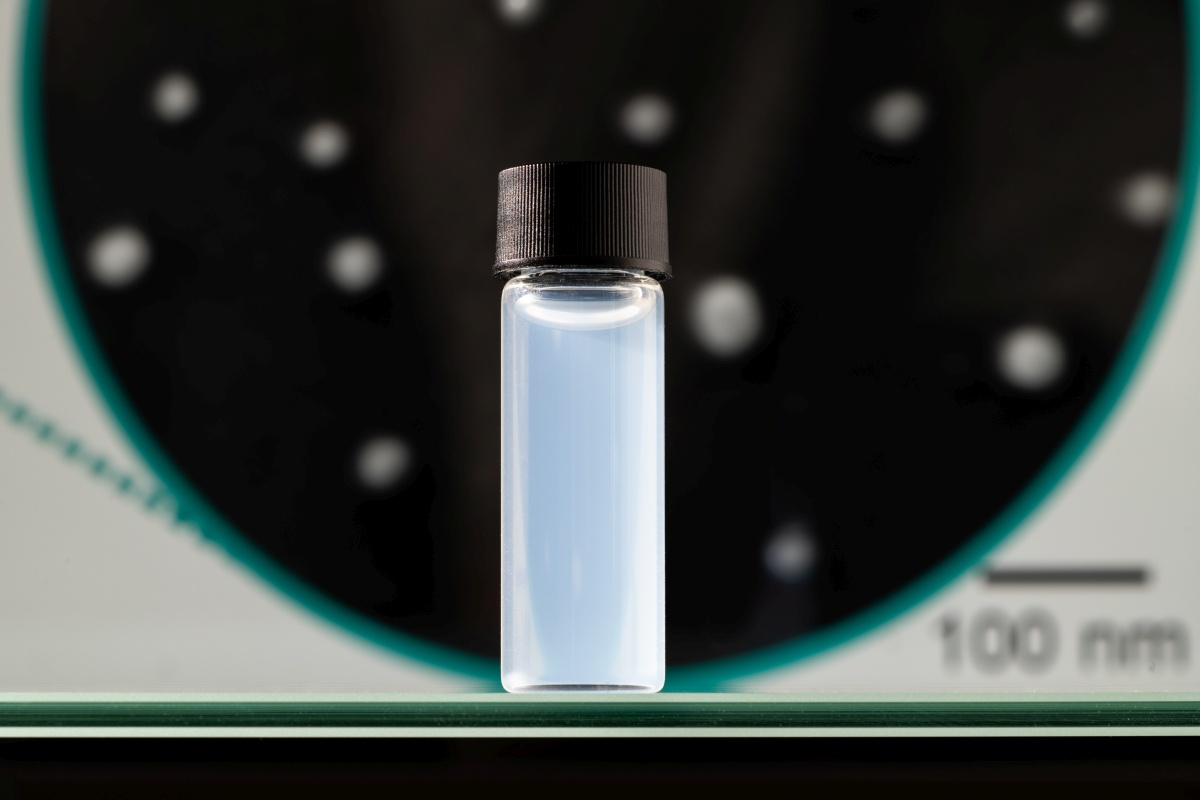
“The nanoparticles we have developed work like a bus,” Feldmann explains. “Filled with cytostatics, this bus moves to where the patient needs the medicine. It stops right near the tumor in the pancreas.” The nanobuses containing the drug are extremely small, i.e. only 20 to 100 nanometers, which is much smaller than a blood cell and even smaller than most viruses.
“Our nanoparticles are able to transport the chemotherapeutic agent gemcitabine directly to the cancer cells in high concentrations,” Alves says. “As a result of this targeted delivery, tumor cells can be fought more effectively and healthy tissue is spared.” Presently, the chemotherapeutic agent is being administered to patients via infusions. The agent then spreads in the whole body. But cytostatics are cytotoxins that inhibit cell division, which is why they may have major side effects in all body regions.
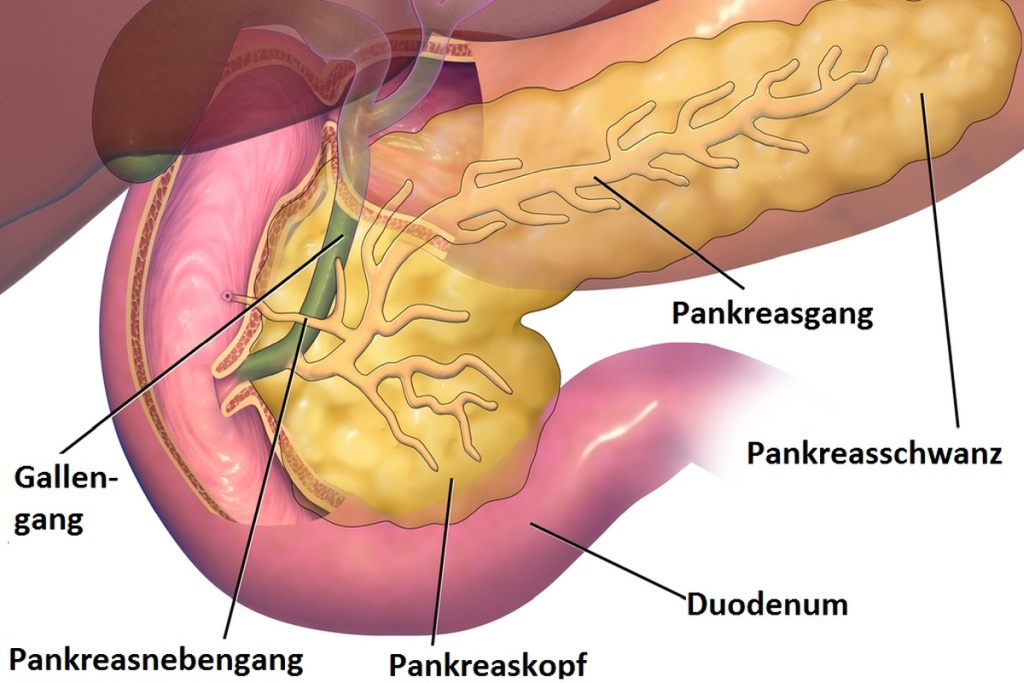
Pancreas
The pancreas is located in the abdomen of humans. It is 15 to 20 cm long. It is an organ of the digestive system, producing digestive enzymes, and regulates blood sugar levels by secreting the hormones insulin and glucagon.
Precise Drug Delivery Thanks to Leaky Blood Vessels
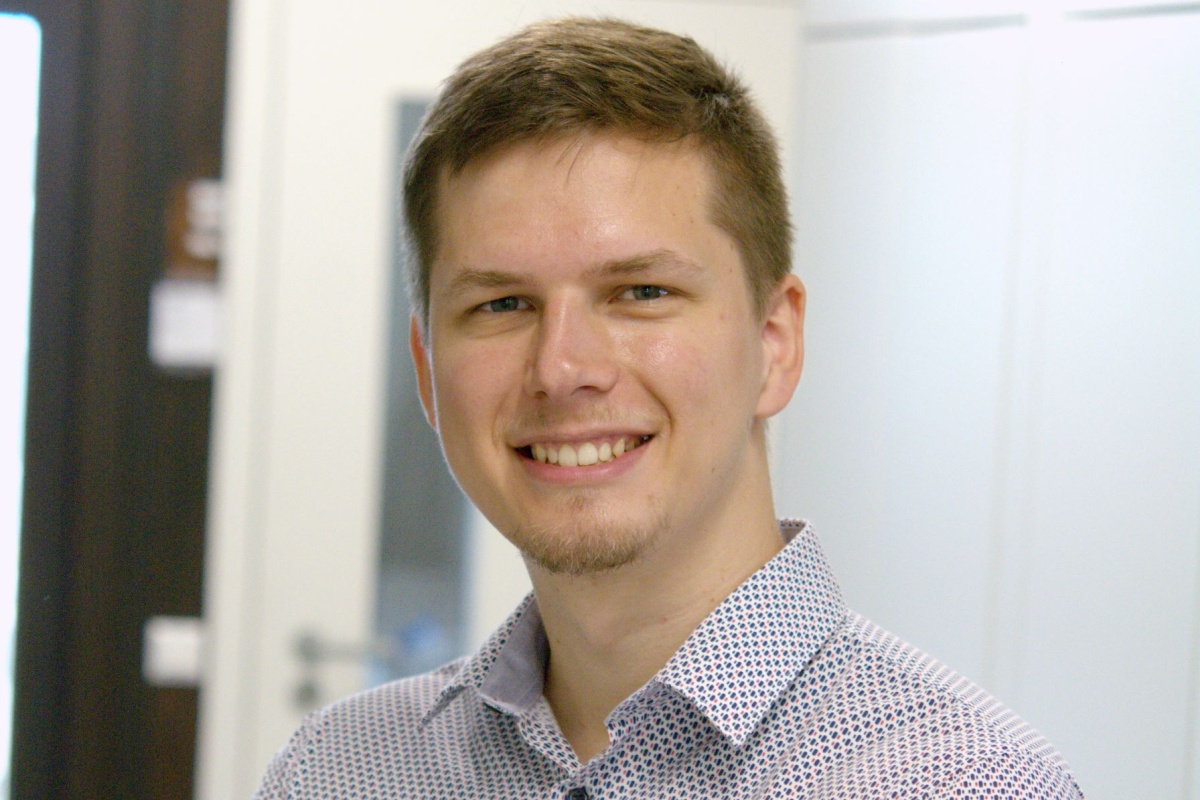
Similar to buses, the newly developed nanoparticles transport drugs directly to the cancer cells, where they will take effect. “Contrary to buses, however, 80 to 90 percent of our loaded nanoparticles consist of the medical agent. And our bus, together with the agent it contains, dissolves completely when it reaches its destination and releases the agent,” explains Dr. David Rudolph, who worked as a doctoral researcher in the group of Feldmann, is now preparing a company to further develop the innovative treatment approach and commercialize the nanoparticles.
The trick with this novel approach is that the blood vessels in tumors differ from those in healthy tissue. Often, they are leaky, which makes it easier for nanoparticles to enter the tumor tissue. This principle has long been known, Alves says. The nanoparticles from the joint project therefore concentrate mainly in tumors and not elsewhere in the body. They remain stuck at their destination and release the drug. “We injected a dye into our nanobus and tracked it by optical imaging in tests with mice. We saw that our particles mainly enter the tumor,” Alves adds. Everything turned out to work as planned.
Hope for a Better Treatment
First research results are highly promising. They give rise to hope for a more effective and less damaging treatment method of pancreatic cancer. Following the first test in mice, the method must be successfully tested in a second animal model before clinical trials on humans can begin.
“Only when we can prove the safety and efficacy of these nanoparticles in humans will it make sense to have them produced on a large scale. And only then will physicians be able to use the method,” Rudolph describes the next steps. Due to legal regulations, researchers expect that it may well take another five years until the method will be used by hospitals. The costs, in particular of clinical studies, will amount to some two to five million euros, although already approved medical agents are used.
“In the long term, this technology could also be adapted for the treatment of other types of cancer,” Feldmann is confident. This would be a real milestone in the fight against this widespread disease.
Martin Grolms, July 11, 2024
Translated by Dipl.-Übers. Maike Schröder